Helpful Tips for New Oncology Patients
As part of our commitment to supporting you during your cancer journey, we offer new patients the opportunity to receive a friendly and informative phone call from a Hope & Cope representative. Hope & Cope is a non-profit organization that provides emotional support and practical resources to help individuals cope with cancer and regain a sense of control and well-being.
More information on Hope & Cope is available in this guide. If you would like to receive this welcome call, please contact 514-340-8255.
Some tips if you are seeing an oncologist / hemato-oncologist (a doctor who specializes in cancer) for the first time:
Everyone has their own way of absorbing information, so choose the one that works best for you. For example you can ask your doctor or nurse to make notes of the key points, or to draw you a diagram, or to record the session. If you want to make a recording of your meeting, ask permission first. There are no “silly” questions. Feel free to ask anything on any subject.
- Researching information
- It might be helpful for you to read some background information about your diagnosis and proposed treatment. Hope & Cope’s library is a good starting point, with a selection of books and pamphlets. Its services are also available online,
 www.hopeandcope.ca/ to learn more. Patient resource center. 514-340-8222 ext. 22438 or 23277 or email
www.hopeandcope.ca/ to learn more. Patient resource center. 514-340-8222 ext. 22438 or 23277 or email  library.jgh@mail.mcgill.ca. Located in JGH Henry Kravitz Library.
library.jgh@mail.mcgill.ca. Located in JGH Henry Kravitz Library.
- It might be helpful for you to read some background information about your diagnosis and proposed treatment. Hope & Cope’s library is a good starting point, with a selection of books and pamphlets. Its services are also available online,
- Preparing questions
- Make a list of questions for your doctor. Someone might be able to help you prepare this list.
- Prioritize your questions, starting with the most important, in case time for your visit is limited. Separate your list into two categories: questions you absolutely need to have answered at this visit, and
questions that can wait until another visit. - Ask for less or more information than the oncologist is prepared to provide. It all depends on how much you feel comfortable receiving at any one time.
- Arrange for company
- It would be helpful to have someone with you and act as “another pair of ears”.
- Don’t be afraid to ask for help from family, friends, medical staff, etc.
- Take notes
- a. Have paper and a pen or telephone to take notes
- b. Keep a diary or list of:
i. all appointments and treatments
ii. the information you receive during your visit with the oncologist
iii. medications/doses and dates
- You may need other tests, such as scans, x-rays and blood work. This is all part of the normal preparation that each person experiences. If you are being seen in the clinic and are coming from home for these tests,
to save your energy, ask whether you might have some of these tests on the same day.
- As part of your treatment, you may be asked to participate in a research study. You are not obligated to agree, but your involvement would be appreciated. Before agreeing, be sure you understand what you will
be asked to do.
- Continue to see your family doctor for any problems that are not related to your cancer.
- Remember that each person’s situation is different, and each case is unique. Two people with the same type of cancer may have different treatment plans.
Ask your pharmacist for a list of the medications you are taking (including all vitamins, natural products, herbs, etc.) and give it to your doctor. Bring a list of any other medical conditions you may have, such as diabetes or allergies. If you are admitted to the hospital, the hospital pharmacist will review your medications.
If having treatments in the out-patient clinic, try not to schedule any other appointments. Sometimes the clinic runs late, so your visit may take longer than expected.
Helpful tips for before starting treatment
- If possible, see your dentist before you start your treatment. Some treatments can lower your body’s ability to fight infection, dental work can increase risk of infection.
- Treatments can make you feel tired. Try to fill up your freezer with food for those days.
- You may be prescribed medications that you take by mouth. Your community pharmacist will explain the possible side effects, and your follow up will be with the doctor.
Treatments while in hospital or in the oncology clinic
- Bring an enjoyable book or headphones with relaxing music to help pass the time while you are waiting for treatment or actually receiving treatment. You will have access to hospital WIFI.
- Before you have treatment, a blood test will be done.
- If you are an in-patient the blood tests are done the day before the treatment
- If coming to the clinic: this is done the day before your treatment in the Oncology Department on the 7th floor of Pavilion E. If you have a central line (a catheter that is placed in a large vein) your blood tests are done on the 8th floor.
- On the day of your first treatment, your nurse will explain your treatment plan, possible side effects, and offer advice.
- When you are coming to the clinic, you will be given a list of emergency phone numbers in case you have any problems outside regular clinic hours. A member of your nursing team will be available for questions or concerns between clinic visits.
- In the clinic , you will receive a pillow and blanket for your chair, and you can close the curtain to take a nap or for privacy. A “light lunch” will be served however you can bring in your own snacks.ill be served around 12:15 p.m.
Please do not bring any valuables when you come for your treatment.
General tips for coping
We know this isn’t easy, but you are not alone. What you’ll find below are simply suggestions. Eventually, you’ll figure out which of them are helpful, and what works best for you. Remember to be kind to yourself and spend time with those you love. Do what makes you happy.
Reach out and connect
- Try to spend time with friends and family who care about you .
- Join a group where you can talk with others who are going through the same thing and will understand how you feel.
- Don’t shut yourself away—being around others can lift your spirits.
- You might like to join a “Look Good, Feel Better” workshop.
Click here (https://lgfb.ca/en/workshop/register-workshop) for more information.
here (https://lgfb.ca/en/workshop/register-workshop) for more information.
Keep doing the things you love
- Laugh when you can using humour help lighten your mood.
- As much as possible, carry on with your usual routines and work. As best you can, stay involved in activities that matter to you.
Get involved
- The more you know, the more in control you may feel.
- Ask information about your diagnosis and treatment.
Do what feels right to you
- Exploring what brings you peace, whether that’s prayer, meditation, or just quiet moments, can help you feel calmer and stronger.
HEMATOLOGY AND ONCOLOGY CLINIC DIRECTORY
Important numbers and locations
Pavilion E, 7th and 8th floors
| Resource | Location | Phone number |
| Reception – Oncology Clinic | Room E-776.2 | 514 340-8248 |
| Reception – Oncology Treatment | Room E-884 | 514 340-8222, ext. 27491 |
| Reception – Pulmonary Oncology | Room E-1055 | 514 340-8225, ext. 23030 |
| Blood Testing | Room E-778 | N/A |
| Hope & Cope | Room E-730.1 | 514 340-8255 |
| Hope & Cope Wellness Centre | 4635, Ch. Côte Sainte-Catherine | 514-340-3616 |
| Oncology Pharmacy | Room E-881 | 514 340-8222, ext. 25940 |
| Nurses’ Office | E-884 | 514 340-8222, ext. 25529 |
| Reception - Hematology | Room E-776.2 | 514-340-8207, ext. 25066 |
If an Infirmière pivot/Nurse Navigator in Oncology (IPO) is assigned to you, that person will give you his/her direct phone number.
YOUR ONCOLOGY TEAM
Many professionals are available to help you, including specialized nurses, social workers, pharmacists, dieticians, Hope & Cope and community services. Many of these roles are explained below
DIETICIAN
While receiving treatment, if you experience weight loss and have side effects that have affected your appetite, please contact your nurse and they will see whether you need a referral to the dietitian.
Well-nourished patients have a better tolerance for cancer treatment, and they seem to recover more quickly from the side effects. For tips see booklet “ Eating well when you have cancer” from the Canadian Cancer Society at: ![]() https://cancer.ca/en/cancer-information/resources/publications/eating-well-when-you-have-cancer.
https://cancer.ca/en/cancer-information/resources/publications/eating-well-when-you-have-cancer.
HOPE & COPE
Main office:
Monday through Friday, 8:00 a.m. to 4:00 p.m.
Wellness Centre: Monday through Thursday, 9:00 a.m. to 5:00 p.m.
Please call 514-340-8255, or visit the website here![]() http://www.hopeandcope.ca/ to learn more and request support.
http://www.hopeandcope.ca/ to learn more and request support.
Hope & Cope offers a wide variety of volunteer-based support and information programs for cancer patients and their families. These include peer mentoring (phone buddy), coping skills classes (The Art of Coping), support groups, after-treatment programs, hospital visits and community referrals. On the 7th floor of Pavillion E you can also find our library and our boutique, where we provide wigs, turbans, scarves, and prostheses free of charge. Hope & Cope also offers free programs such a as yoga, art, Tai Chi, acupuncture and many more. The gym and and its courses are available for you and your family/caregivers. Through this journey, Hope & Cope is there for you. Its website(![]() www.hopeandcope.ca) features a monthly calendar, as well as listings of upcoming lectures and events.
www.hopeandcope.ca) features a monthly calendar, as well as listings of upcoming lectures and events.
Please call about anything that interests you, 514-340-3616.
McGILL CENTRE FOR TRANSLATIONAL RESEARCH
This centre gives you an opportunity to participate in early-phase clinical research. Patients are referred by their oncologists when this involvement is clinically indicated. More information can be found on its website: ![]() https://www.mcgill.ca/translational-research-cancer/.
https://www.mcgill.ca/translational-research-cancer/.
NURSE
The Segal Cancer Centre has a comprehensive nursing care team whose members specialize in cancer care.
The nursing teams can also provides you with teaching, counselling and support related to cancer and your treatments . The nurse’s role includes:
- evaluating the impact of the illness on you and your family
- explaining and providing information about your treatment (chemotherapy/immunotherapy), possible side effects, and how to take care of symptoms related to the illness or medications (e.g., nausea, vomiting, fever, pain, constipation, diarrhea)
- administering your treatment (chemotherapy/immunotherapy) and/or medications
- following up to determine how you are coping physically and emotionally responding to your varying needs by consulting with or referring you to other healthcare professionals (e.g., dietician, Hope & Cope, social worker, psychologist, psychiatrist, supportive care team, CLSC)
Infirmières pivots in Oncology (IPO)
Are oncology nurse clinicians, who work closely with the other healthcare professionals on your care team (those in hospital and in the community). You might be assigned an Infirmière pivot in Oncology (IPO), depending on your needs, type of cancer and diagnosis. The IPO helps guide you throughout your experience with cancer by assessing you needs and symptoms, providing information, teaching, offering support and coordinating your care within the healthcare system. You may see them in person or speak with them at different points in your cancer care journey.
Nursing team for the in-patient units
These nurses have additional training and certification to give anti-cancer treatments. They support you and your family with information and help with the side effects.
Nursing team for out-patients
The team is available Monday through Friday from 8:00 a.m. to 4:00 p.m., in person, or by phone. You will meet a nurse each time you come to the clinic for treatment. Nurse clinicians are also available to you on the Symptom Management Hotline, at 514-340-8222, ext. 25529 (8:00 a.m. to 4:00 p.m., Monday through Friday) if you are having any side effects.
NURSE PRACTITIONER (NP)
Nurse practitioners in hematology-oncology work alongside your hematologist s to assess, diagnose, and manage your treatment. They perform physical exams, order and interpret tests, prescribe medications as well as monitor for side effects and treatment response. NPs also educate patients and families about diagnoses and care plans, provide emotional support, and help coordinate services across the healthcare team. In addition, they assist with follow-up, ensuring patients receive comprehensive, continuous support throughout their cancer journey.
OCCUPATIONAL THERAPIST (OT)
The OT helps you resume the activities of daily living through rehabilitation.
OMBUDSMAN
The ombudsman is available Monday through Friday from 9:00 a.m. to 5:00 p.m. at 514 340-8222, ext. 24222, or via email at: ombudsman.CCOMTL@ssss.gouv.qc.ca It is essential for JGH patients to be able to voice their dissatisfaction and to comment in a confidential manner about the care they have received. To do so: • First speak with a member of your healthcare team, who will try to correct the problem or find a solution to the matter you have raised. Depending on the circumstances, the team member may direct you to the appropriate person. • If the problem persists, contact the Office of the Commissioner of Complaints and Quality of Service at the phone number above or at ombudsman.ccomtl@ssss.gouv.qc.ca. More information about the complaint process is available here.
ONCOLOGIST
Hematologists and oncologists are doctors who specialize in cancer and determine the type of treatment you may need to follow. They will examine you and explain your treatment. Throughout treatment, they will perform follow-ups with you; they will also follow you once your treatment has ended.
They see patients by appointment in their clinic from Monday to Friday. If you are admitted to hospital, they will be taking care of you while in hospital and then follow you as an out patient.
PHARMACIST
Monday through Friday, 8:00 a.m. to 4:00 p.m.
The pharmacist works with the oncology team to make sure you receive the drugs that are used in your treatment, help you manage side effects, and provide you with information about your treatment. Pharmacists also counsel patients about drug-related matters, such as chemotherapy, side effects, drug interactions, pain management and symptom control. In addition, they dispense the drugs that are ordered by the doctor for your treatment.
PHYSIOTHERAPIST
The physiotherapist can help you perform exercises to strengthen the muscles that are affected by surgery, treatment or the disease itself.
PSYCHOLOGIST / PSYCHIATRIST
If you are having a hard time dealing with your diagnosis and/or treatment, the services of a psychologist and psychiatrist are available to you. Your nurse, doctor or social worker can make the necessary referrals.
RECEPTIONIST
Among the tasks that the receptionist performs is making appointments for tests (such as x-rays and scans) and follow-up visits. You must check in with the receptionist when you arrive for an appointment of any kind at the clinic. They do not provide any medical test results. If you are having a medical problem, do not speak with the receptionist; instead, talk with your nurse.
ONCOLOGY CLINIC FOR SENIORS
This special program is designed to serve the needs of older adults with cancer. Your doctor may refer you to this team if needed
SOCIAL WORKER
Monday to Friday, 8:30 a.m. to 4:30 p.m., at 514-340-8240
The social worker helps to boost the strength of individuals or family members as they cope with the stresses caused by cancer. Through counselling, and by linking with hospital and community resources, they support you and your family/caregiver.
STUDY COORDINATOR
Some patients may participate in a clinical trial or research study, which is coordinated by a study coordinator This person provides instructions about such matters as follow-up appointments and the scheduling of tests.
SUPPORTIVE CARE TEAM (S.C.T.) / Palliative Care
The objective of the Palliative Care/Supportive Care team is to meet the physical, psychological, social and spiritual needs of patients. The team helps manage your symptoms throughout the cancer trajectory, and not only during end-of-life care. The S.C.T. specializes in controlling pain and symptoms (e.g., nausea, vomiting, constipation) and off ering emotional support to you and your family/caregiver. The S.C.T. stays in contact with you by phone (when you’re at home), in the hematology/oncology clinics, and when you’re admitted to the hospital. Your nurse can refer you to this team.
The McGill Cancer Nutrition Rehabilitation Program
The Cancer Nutrition Rehabilitation (CNR) team at the Jewish General Hospital has the goal of improving your nutrition, physical function and overall quality of life. Working with you, your family or caregivers and your treating oncology team, we aim to help patients with cancer experiencing weight loss, decreased appetite, reduced physical function, and fatigue or weakness. The core CNR clinical team includes a physician, nurse, a physiotherapist and a dietitian. If you are experiencing these symptoms, please ask your treating team for a referral to our program.
Symptom Tip Sheets
We have created 19 one-page tip sheets for common Symptoms that you might experience. These could help you as you begin treatment. All of the tip sheets can be found here, see the Symptom Tip Sheets page.
| SYMPTOMS: | |||
|---|---|---|---|
| Pain | Fatigue/ Tiredness | Nausea/ Vomiting | Appetite loss |
| Shortness of breath | Depression | Anxiety | Constipation |
| Sleep changes | Diarrhea | Mouth Sores | Mouth Dryness |
| Skin rash | Bleeding | Peripheral neuropathy | Body image |
| Coughing | Preventing falls | Relaxation exercises | Exercises de relaxation |
| Includes additional information on : Physical Symptoms, emotional symptoms, practical, Informational, spiritual, social and family. | |||
Symptom Management Hotline

The Symptom Management Hotline at the Jewish General Hospital allows out- patients who are experiencing side effects related to treatments or cancer to contact our cancer care nurses between 8:00 a.m. and 4:00 p.m., Monday through Friday. The Symptom Management Hotline nurse will assess you over the phone and develop a care plan for the symptoms you are experiencing.
Please call immediately if you have a fever over 38°C (100.4°F), taken by mouth. If have fever outside of the working hours, please go to the Emergency room.
Treating cancer with chemotherapy can lead to a number of side effects, such as nausea, vomiting, fever, weakness, fatigue, skin reactions and problems in the digestive system. These can be quite severe and they often lead to visits to the Emergency Department. If you experience side effects related to your treatment, please call the Hotline as soon as possible to help avoid a trip to the hospital. In many cases, all it takes is a phone call.
If, for any reason, you must visit the Emergency Department, please remember the following:
- Tell the triage nurse you are a cancer patient.
- Provide the name of your oncologist.
- Bring your oncology passport or a list of your medications, including the type of cancer treatment you are receiving.
Links to educational videos
- Introduction to the
 JGH Segal Cancer Centre
JGH Segal Cancer Centre  Virtual Tour of the Segal Cancer Centre
Virtual Tour of the Segal Cancer Centre Guide to chemotherapy
Guide to chemotherapy Guide to immunotherapy
Guide to immunotherapy Guide to cancer nutrition
Guide to cancer nutrition Guide to surgery
Guide to surgery Coping during COVID-19
Coping during COVID-19- Guide to radiation therapy (Note: This video may not apply to you. Please check with your healthcare professional):
NOTE: All of the Precare videos are available in 18+ languages. Simply click on the “CC” button on the bottom right of the screen and choose the language:
Other Resources:
HOPE & COPE’S SERVICES
Supporting patients and their families throughout the cancer journey
Why me? What now? These are just some of the questions after cancer is diagnosed. Hope & Cope’s cancer-experienced volunteers, supervised by members of the professional staff , off er a wide variety of bilingual programs and services free of charge to patients and their families. These services are available at the Jewish General Hospital (in Oncology, Radiation Oncology and Palliative Care) and at the JGH Hope & Cope Wellness Centre.
Many of services are also offered online. Click ![]() here for the calendar.
here for the calendar.
- Cancer Exercise and Rehabilitation Program – physical evaluations and individualized exercise programs
- Clinic volunteers (Oncology, Radiation Oncology) support you while you receive treatment.
- Creative therapies, including choir, art, jewellery-making and more
- En famille – a program for families with children up to age 18, in which a parent has cancer
- Energy work – Reiki, etc.
- Library – books, pamphlets, computers for patient and caregivers’ use
- Look Good, Feel Better – workshops on skin care, make-up techniques and head coverings
- Nutrition lectures, cooking classes and interactive workshops
- Palliative care and bereavement – including mentors and support groups, hospital visits, peer mentors,
- Peer mentoring – linking you with a volunteer who underwent a similar cancer experience
- Relaxation, meditation and physical activities, such as yoga, qi gong, tai chi
- Support groups for general and specific cancers
- “The Art of Coping” – for stress management ; “Mindfulness and Self-Compassion”
- Transitional programs, such as Focus on the Future “Life After Cancer”, to help you move forward after treatment
- Wigs, head coverings and scarves
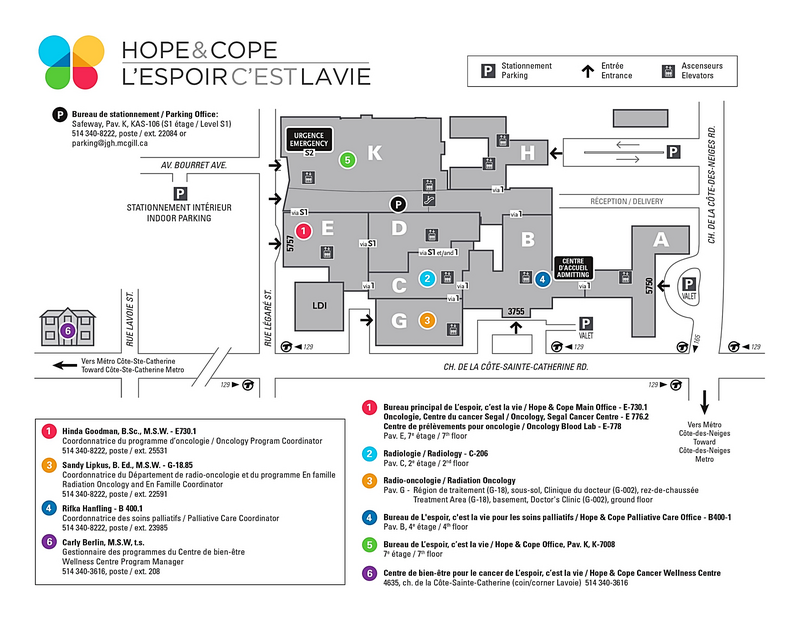
Hope & Cope – Main Office
3755 Côte-Saint-Catherine Road
Room E-730.1 (Pavilion E, 7th floor)
Montreal, QC H3T 1E2
514-340-8255![]() https://hopeandcope.ca/
https://hopeandcope.ca/
Hope & Cope Wellness Centre
4635 Côte-Saint-Catherine Road
(Corner Lavoie)
Montreal, QC H3W 1M1
514-340-3616![]() hopecope@jgh.mcgill.ca
hopecope@jgh.mcgill.ca
Wellness questionnaire
Your health care team would like to better understand how you are feeling, your concerns and symptoms throughout your treatment. When you are an out-patient, you will be asked to fill in the ![]() Wellness questionnaire 48 hours before your treatment appointment.
Wellness questionnaire 48 hours before your treatment appointment.
This will help us improve your quality of care and communication with your team, and decrease symptoms. Please fill out the ![]() Wellness questionnaire, or via the email link we sent you. If you have questions reach out by email to
Wellness questionnaire, or via the email link we sent you. If you have questions reach out by email to ![]() jgh.oncologysurveys.ccomtl@ssss.gouv.qc.ca.
jgh.oncologysurveys.ccomtl@ssss.gouv.qc.ca.
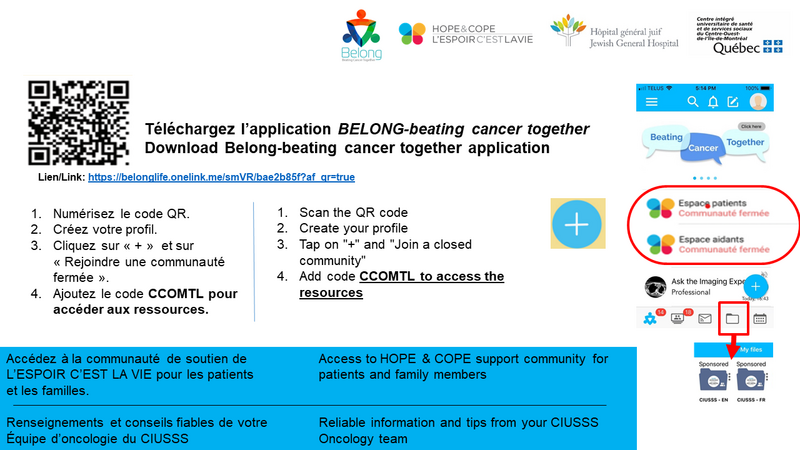
Belong App
Belong app offers patients, family and friends bilingual information, resources, and support about and throughout the cancer care journey. In the Belong app, the CIUSSS Segal Cancer oncology team has included:
- Area for patients and family members/ caregivers to chat and get peer support, and support from Hope & Cope
- Information, educational videos including orientation folder, nutrition videos, tour of the Segal cancer, symptom management tip sheets and more
- Resources in the community & reliable websites (Look good feel better, Canadian Cancer Society, Foundation Quebecoise du cancer, Cancer and Work, transportation and finances, etc.)
To have access to these areas on the ![]() web or on your mobile device:
web or on your mobile device:
 download the app on your mobile device
download the app on your mobile device- create your profile
- add the code CCOMTL
See detailed instructions below:.
PARKING AND TRANSPORTATION
New government regulations allow for free parking for the first 2 hours in the underground parking lot beneath Pavilion K. Spaces are limited, first come first served.
AFTER 2 HOURS, THE RATES ARE:
- 2 h - 3 h 59 min: $ 3.25
- 4 h - 24 h: $ 5.50
Ask the receptionist for the form required, and have your hospital card with you.
YOU CAN BUY A PARKING PASS FROM PARKING OFFICE FOR:
- Outpatient: $ 24.75 for one week or $ 49.75 for one month
- Inpatient: $ 51.00 for one week or $ 102 for one month
The parking office is in Pavilion K, S1 (room KAS 106) near the security desk just inside the Legare entrance.
Hope & Cope may be able to help you find community or private driving resources. Please drop by room E-730.1 (Pavilion E) or call at 514-340-8255ce.
---------
Need a family doctor:
call 811 option 3
Need help to stop smoking:![]() iquitnow.qc.ca or 1 866 527 7383
iquitnow.qc.ca or 1 866 527 7383